why charcoal
five good reasons to use charcoal
When you are sick, suffering pain, or battling some infection, why should you first consider a simple and natural remedy like medicinal charcoal instead of pharmaceutical drugs?
There are at least FIVE good reasons why you should not choose pharmaceutical drugs as your first line of treatment.
Five Good Reasons
Not to Choose Pharmaceutical Drugs
- Adverse Effects - too numerous to count
- Iatrogenic Death- over 251,000 annually (year 2016) - the cure is more deadly than the disease.
- Nosocomial Infections - over 110,000 annually (year 2016)
- Drug Viability & Availability - unreliable in times of disaster, pandemics & war
- Cost - over $5680 annually per man, woman & child(= $26 billion)
Five Good Reasons
To Choose Medicinal Charcoal
Reason #1 Charcoal is Affordable
- For the wallet and for the body
- For whatever currency, whatever culture
Reason #2 Charcoal is Easy
- Easy to make
- Easy to take - orally
- Easy to apply - as a poultice or bath
- Requires no dictionary, prescription, license or degree
Reason #3 Charcoal WORKS
- For poisoning, drug overdose, and food poisoning
- For digestive, and other gastro intestinal problems such as acid reflux, diarrhea, nausea, vomiting and gas
- For poisonous bites: including bees, hornets, brown recluse spiders, scorpions, and poisonous snakes
- For allergic reactions to poisonous plants such as poison ivy and poison oak
- For infections: including pink eye, diabetic ulcers, abscesses, UTI, and gangrene
- For diseases such as Gout, Tourista, tetanus, diptheria, and cholera
- For animals: including poisoning, infections, odors, and as a digestive supplement
- For purifying water, air and food
- and more...
Reason #4 Charcoal is SAFE
- A safety record that goes back 3500 years
- Rated Category 1 (Safe and effective by the FDA)
- Recommended by Poison Control Centers, Pediatric & Toxicologist Associations
- Has no known adverse side effects
- Non habit forming
- Indefinite shelf life - does not age or spoil if properly stored
Reason #5 Charcoal is ACCESSIBLE
- Universally available around the world
- In hospitals, clinics, pharmacies, and healthfood stores
- In the city, in the country
- In disasters, calamities, times of war
iatrogenic death
“Iatrogenic”, from the Greek Iatros meaning “physician” and -genic, meaning “induced by” – together “physician-induced”. Medical definition: “induced by a physician’s words or therapy (used especially of a complication resulting from treatment).” Thus Iatrogenic death is death resulting directly or indirectly from a physician’s words or therapy.
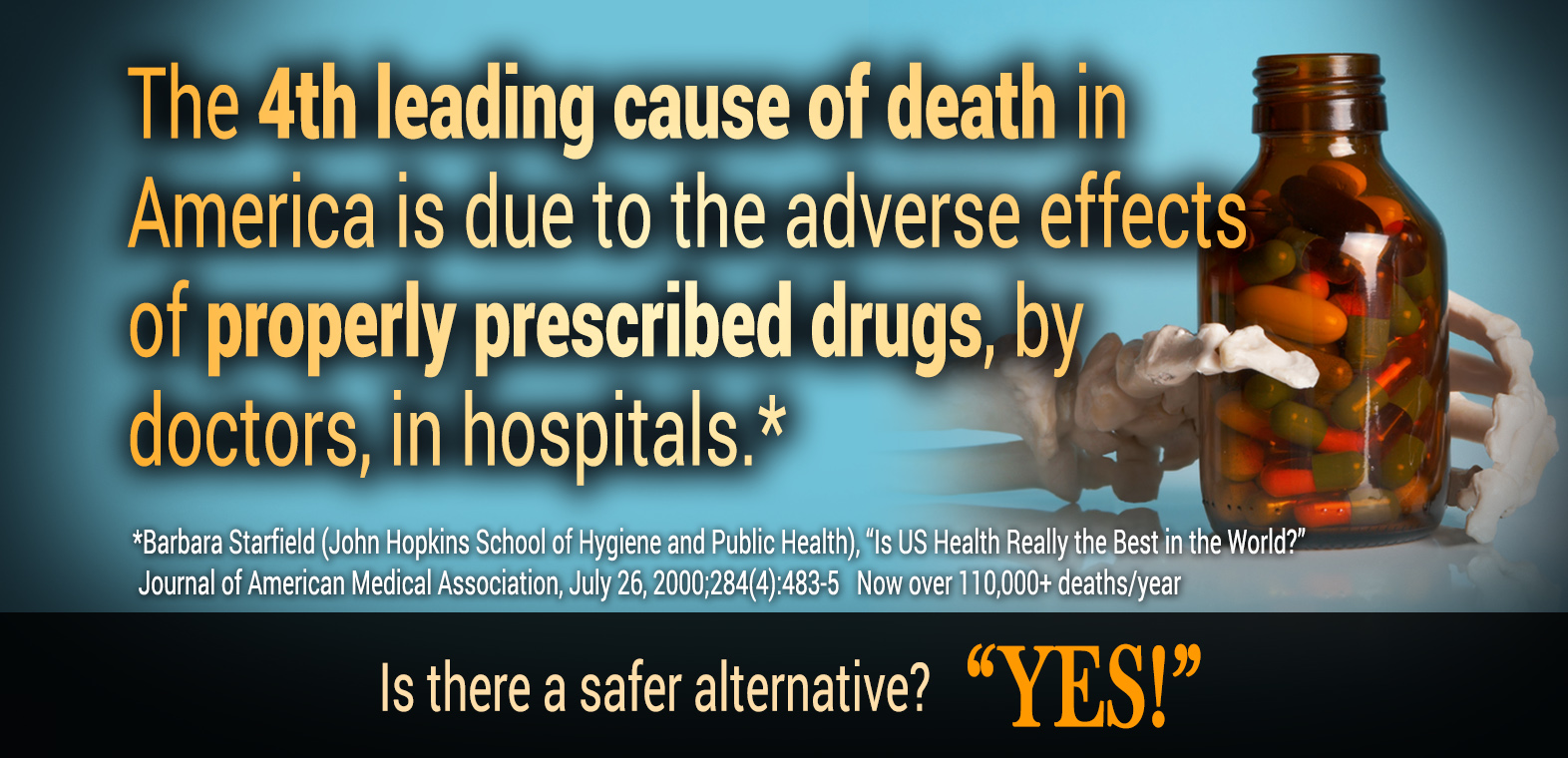
In 2000, a presidential task force labelled medical errors a “national problem of epidemic proportions.” Members estimated that the “cost associated with these errors in lost income, disability, and health care costs is as much as $29 billion annually.” In the same year the Journal of the American Medical Association published a study by Dr. Barbara Starfield (John Hopkins School of Hygiene and Public Health) that put Iatrogenic deaths in America at the astounding number of 225,000!
Dr. Starfield cautioned that as startling as this research was, it only represented hospitalized patients – it did not include deaths in nursing homes, emergency rooms, or in doctor’s offices. It did not include negative effects that are associated with disability or discomfort. And, these estimates of death due to error are lower than those in other published reports (L. Leape -1997). Nevertheless, 225,000 iatrogenic deaths per year constitute the third leading cause of death in the United States, after deaths from cancer and heart disease! The most significant number of these unnecessary deaths, 106,000, were due to the negative effects of properly prescribed drugs, making them the fourth leading cause of death in America.
Total deaths due to medical error 225,000
Total cost $100 Billion
1997 estimated total deaths due to medical error 420,000
1997 total estimated cost $200 billion
2016 Update
7 Most Deadly Surgeries JAMA Surgery (April 27, 2016)
In an analysis of 421,476 patient records from a national database of hospital inpatients, researchers discovered that a mere seven procedures accounted for approximately 80 percent of all admissions, deaths, complications and inpatient costs related to emergency surgeries. The sample included only adults who underwent a procedure within two days of admission from 2008 to 2011.
The seven dangerous and costly procedures are mostly related to the organs of the digestive system:
- Removing part of the colon,
- Small-bowel resection,
- Removing the gallbladder,
- Operations related to peptic ulcer disease,
- Removing abdominal adhesions,
- Appendectomy
- Other operations to open the abdomen.
50% of Surgeries have Drug Error at Top U.S. Hospital (Anesthesioology October, 2015)
Researchers at Massachusetts General Hospital found that 124 of the 277 operations they watched in 2013-2014 included at least one medication error or drug-related incident that harmed a patient. Among the most frequently observed errors were mistakes in labeling, incorrect dosages and medications that should have been given but were not.
More than one-third of the observed errors injured patients, including three life-threatening mistakes, according to the study.
The error rate is much higher than what has been previously reported but in line with rates found in inpatient wards and outpatient clinics, researchers said. There have been a few studies about medication errors in the operating room but they relied mostly on self-reported data, which typically underrepresent true rates.
The medications most frequently associated with errors were propofol, a commonly used sedative in the operating room; fentanyl, a powerful pain medication; and phenylephrine, a medication given to increase blood pressure in patients with very low blood pressure.
On average, about 10 medications were given during an operation. The study found that some kind of error was made in about 1 in 20 medications, which equates to every other operation.
“Boy, we still have a lot of work to do,” said Tejal Gandhi, president and chief executive of the National Patient Safety Foundation. “If it happens at MGH, it can happen anywhere.”
Are you reassured?
Nosocomial
Nosocomial:
1. Of or relating to a hospital.
2. Of or being a secondary disorder associated with being treated in a hospital but unrelated to the patient’s primary condition.
The term “nosocomial” comes from two Greek words: nosus meaning “disease” and komeion meaning “to take care of.” Broadly, “nosocomial” first applied to any disease contracted by a patient while under medical care. However, today it has become synonymous with “hospital-acquired”. In other words, an infection a person acquired at a hospital and not one they had before they arrived.
How seriously do nosocomial infections impact the general public?
| U.S. cases | 2 million annually |
| 3 per minute = 10% American hospital patients | |
| Deaths | 80,000 (JAMA 7/2000) |
| 9 per hour | |
| Cost | $1.71 billion |
The New England Journal of Medicine reported in 1981: “Hand washing is considered the single most important procedure in preventing nosocomial [hospital-borne] infections…[but] compliance of healthcare workers with recommended hand washing practices remains unacceptably low…. We found that, on the average, hospital personnel washed their hands after contact with [intensive care unit] patients less than half the time. Physicians were among the worst offenders.” Sad to say, this practice has not been significantly reversed. And, when a case of nosocomial infection does develop, physicians routinely turn to drugs and antibiotics to try and reverse the failure to follow fundamental rules of hygiene.